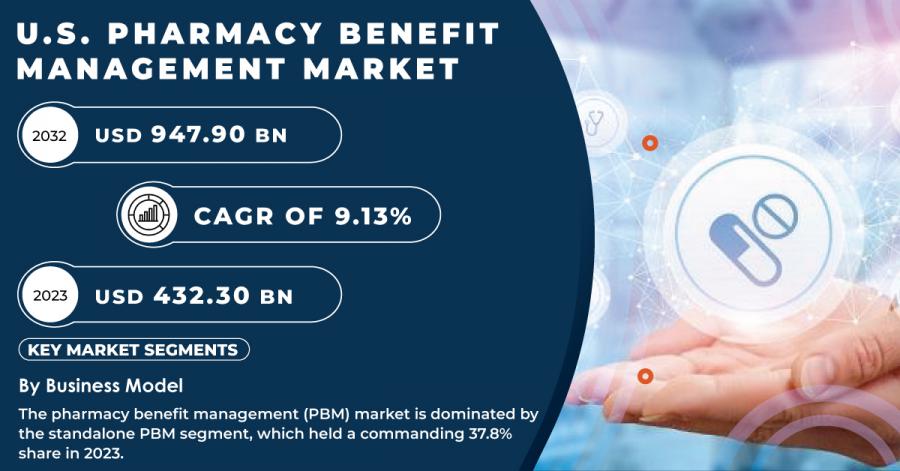
U.S. Pharmacy Benefit Management Market Size to Reach USD 947.90 Billion by 2032, Witnessing a CAGR of 9.13%
The U.S. Pharmacy Benefit Management (PBM) Market is expanding rapidly due to rising prescription drug costs and the demand for affordable healthcare solutions.
AUSTIN, TX, UNITED STATES, December 2, 2024 /EINPresswire.com/ -- The U.S. Pharmacy Benefit Management Market was valued at USD 432.30 billion in 2023 and is expected to reach USD 947.90 billion by 2032, growing at a CAGR of 9.13% over the forecast period from 2024 to 2032.
Growth and Innovation in the U.S. Pharmacy Benefit Management Market: Navigating Rising Healthcare Costs and Advancing Technology
The U.S. Pharmacy Benefit Management Market plays a pivotal role in managing prescription drug benefits for insurers, employers, and governmental health programs. As healthcare costs continue to rise, PBMs are becoming essential in controlling and managing prescription drug spending, making medications more accessible and affordable for patients. They act as intermediaries between pharmaceutical manufacturers and patients, negotiating drug prices, establishing formularies, and ensuring that patients receive appropriate medications at the most affordable rates.
With a rapidly aging population and the increasing prevalence of chronic diseases such as diabetes, heart disease, and hypertension, the demand for pharmacy benefit management services is expected to grow. In response, PBMs are adopting advanced technologies such as artificial intelligence (AI) and machine learning to improve drug cost management and optimize healthcare spending. Furthermore, new regulatory frameworks and transparency initiatives are pushing for increased competition and better service delivery from PBMs, which will drive future market growth.
Get a Free Sample Report of U.S. Pharmacy Benefit Management Market @ https://www.snsinsider.com/sample-request/4407
Key Players:
➢MedImpact
➢Elixir Rx Solutions LLC
➢CVS Health
➢HUB International Limited
➢Cigna
➢Anthem
➢Prime Therapeutics LLC
➢Change Healthcare
➢CVS Caremark
➢Express Scripts
➢OptumRx
Rising healthcare costs, especially prescription drug prices, are mitigated by Pharmacy Benefit Managers who negotiate better prices with pharmaceutical companies to control costs.
Rising healthcare costs, particularly the increasing prices of prescription drugs, have become a significant concern for patients, employers, and insurers. High drug costs place a financial burden on individuals, limiting access to necessary medications and straining insurance systems. Pharmacy Benefit Managers (PBMs) play a crucial role in addressing this challenge by acting as intermediaries between pharmaceutical companies, insurers, and healthcare providers. PBMs negotiate with drug manufacturers to secure lower prices for medications, leveraging their purchasing power to obtain discounts and rebates. This helps reduce the overall cost burden on consumers and insurers by making drugs more affordable. In addition to negotiating prices, PBMs also work to streamline the drug purchasing process, ensuring that medications are available at lower costs while maintaining quality.
Dominance of Standalone PBMs and Commercial Insurance Segment in 2023
By Business Model: The standalone PBM segment dominated with the market share over 37.8% in 2023. This segment comprises PBMs that operate independently and provide services to various clients, including insurers, self-insured employers, and government organizations. Recent mergers and acquisitions involving key players, such as CVS Health and Express Scripts, are further driving consolidation in the market. These strategic consolidations are likely to enhance companies' control over pricing strategies and offer valuable insights into competitors' tactics.
By End-use: The commercial segment dominated with the market share over 64.65% in 2023. This dominance can be attributed to the large number of U.S. employees who are covered by commercial private insurance plans. These plans typically include copay systems that help manage the high costs of medications, making them an attractive option for both employers and employees. As a result, the commercial insurance sector continues to play a crucial role in the healthcare landscape. Additionally, the growing trend of employers offering drug benefit plans as part of employee healthcare packages is expected to further fuel the growth of this segment.
Buy Full Research Report on U.S. Pharmacy Benefit Management Market 2024-2032 @ https://www.snsinsider.com/checkout/4407
Driving Forces of the U.S. Pharmacy Benefit Management Market: Government Influence and Transparency Initiatives
The U.S. Pharmacy Benefit Management Market is largely driven by developments in the commercial and government sectors. The U.S. government continues to play a pivotal role in shaping the market, particularly through Medicare and Medicaid programs, which rely heavily on PBMs to manage prescription drug benefits. Several state and federal initiatives are pushing for increased transparency in drug pricing, which is expected to create both challenges and opportunities for PBMs in the coming years.
Recent Developments
➢In August 2023: The major nonprofit advocacy group AARP, alongside Senators Maria Cantwell and Chuck Grassley, supported the introduction of the Pharmacy Benefit Manager (PBM) Transparency Act. This bill aims to increase transparency in PBM operations and address concerns regarding drug pricing and benefit management practices, potentially reshaping the market landscape.
➢In August 2023: CVS Caremark, one of the leading PBMs in the U.S., announced that it had dropped Blue Shield of California as a pharmacy benefit manager. This decision follows Blue Shield's decision to form a new partnership with another PBM that would offer drug-pricing services at similar rates. The change is expected to influence drug pricing strategies across California and has sparked wider conversations about PBM market dynamics.
Speak with Our Expert Analyst Today to Gain Deeper Insights @ https://www.snsinsider.com/request-analyst/4407
About Us:
S&S Insider is a global leader in market research and consulting, shaping the future of the industry. Our mission is to empower clients with the insights they need to thrive in dynamic environments. Utilizing advanced methodologies such as surveys, video interviews, and focus groups, we provide up-to-date, accurate market intelligence and consumer insights, ensuring you make confident, informed decisions.
Akash Anand
SNS Insider | Strategy and Stats
+1 415-230-0044
email us here
Visit us on social media:
Facebook
X
LinkedIn
Instagram
YouTube
Distribution channels: Healthcare & Pharmaceuticals Industry
Legal Disclaimer:
EIN Presswire provides this news content "as is" without warranty of any kind. We do not accept any responsibility or liability for the accuracy, content, images, videos, licenses, completeness, legality, or reliability of the information contained in this article. If you have any complaints or copyright issues related to this article, kindly contact the author above.
Submit your press release